Contact Lenses after Corneal Transplant

KC and Down syndrome: More Research Needed
March 25, 2024
Health Literacy: Minimal Keratoconus Knowledge
April 10, 2024Originally published in NKCF Update (February 2024).
One mistaken belief by many with keratoconus is that a corneal transplant will cure their disease. Another is that a transplant will result in perfect vision.
Keratoconus is not cured by replacing the cornea. There are even some reports of disease progression after transplant surgery. The treatment that halts disease progression is corneal crosslinking, not a transplant.
Another misunderstanding is that a cornea transplant results in precise 20/20 vision. While in many cases, people with severe keratoconus can get by with eyeglasses after surgery, it is not unusual or a sign of failure on the surgeon’s part if a patient must rely on contact lenses to correct and optimize vision after a transplant.
Dr. Jamie Kuzniar OD of Rochester Hills, MI is co-author of a recent article on the subject. In it, she reminds doctors of the steps they should be taking for patients referred for contact lenses after corneal transplant surgery.
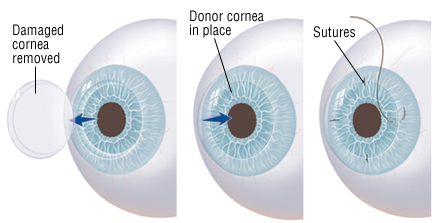
Most patients who undergo a full corneal transplant have a recovery period of 4 to 6 months, where the eye surgeon is regularly checking on healing and intermittently removing sutures that hold the graft in place. Removal of sutures can lead to small vision changes, so this may delay contact lens fitting.
Dr. Kuzniar emphasized the importance of thorough eye exams, looking for any signs of graft rejection or irritation when these patients are sent for contact lens fitting. New, tiny blood vessels visible on the eye may be signs of neovascularization and need attention.
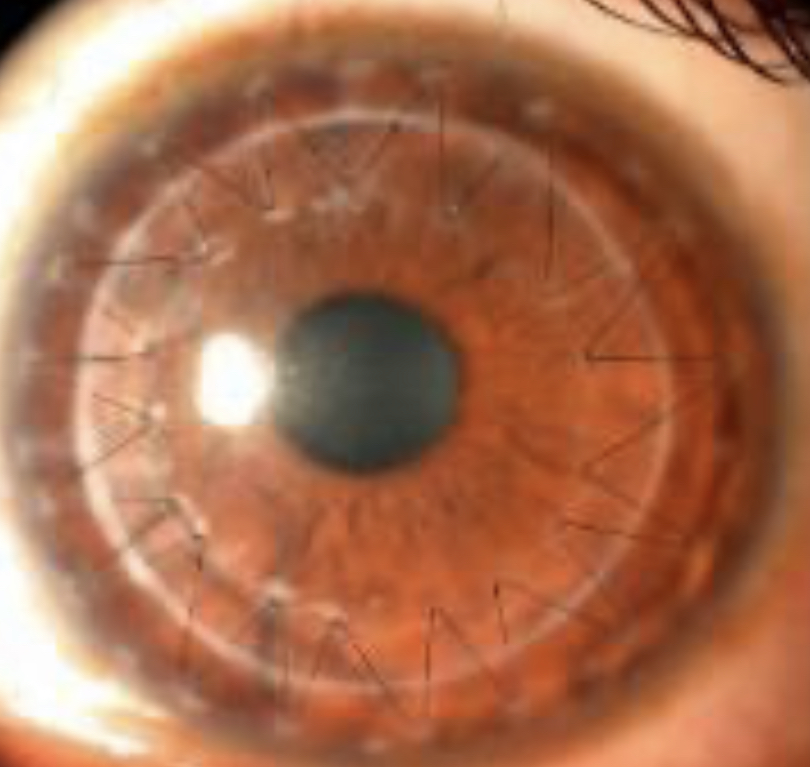 Any new haze or scarring should be documented. Lifting or sinking of the graft will also be of concern. Your doctor may also conduct a cell count to check the overall health of the transplant.
Any new haze or scarring should be documented. Lifting or sinking of the graft will also be of concern. Your doctor may also conduct a cell count to check the overall health of the transplant.
Your contact lens fitter will likely rely on two types of lenses: gas permeable (GP) cornea lenses or scleral lenses, which are larger in shape and allow the graft to be immersed in liquid nutrients.
Before selecting a contact lens type, your doctor will want to discuss your vision needs and will consider what type of lenses you may have worn in the past. Your doctor will also look at the size and placement of the graft. That may determine which type of lens will work best. Your contact lens fitter will want to find a lens that does not irritate the junction between your own cornea and the replacement graft. Your doctor will want to avoid anything that sits too heavily on the graft or a lens that will move around the eye causing irritation.
The number of cornea transplants for keratoconus decreases each year. Factors include earlier diagnosis and treatment, and the availability of better contact lens options. At one time, patients with moderate to severe disease would be candidates for a corneal transplant. Now most live their lives without undergoing surgery and reply on contact lenses to improve vision and eye health.
Reference: Messer BM, Fosso T, Kuzniar J, Contact Lens Wear After Corneal Transplantation, Contact Lens Spectrum, 34-41, October 1, 2023.
 Dr. Jamie Kuzniar OD, FSLS, FAAO is a graduate of the Michigan College of Optometry. She completed a corneal disease and contact lens residency at Indiana University and is a Fellow of both the American Academy of Optometry and the Scleral Lens Education Society. Dr. Kuzniar is owner and founder of Elevate Eye Care and Eyewear in Rochester Hills, Michigan, where she specializes in fitting specialty contact lenses for patients with keratoconus.
Dr. Jamie Kuzniar OD, FSLS, FAAO is a graduate of the Michigan College of Optometry. She completed a corneal disease and contact lens residency at Indiana University and is a Fellow of both the American Academy of Optometry and the Scleral Lens Education Society. Dr. Kuzniar is owner and founder of Elevate Eye Care and Eyewear in Rochester Hills, Michigan, where she specializes in fitting specialty contact lenses for patients with keratoconus.