Who is Not a CXL Candidate?

Keratoconus & Pregnancy: a case for pro-active CXL
September 23, 2019
COVID-19 and Corrective Lens Wear
March 17, 2020Since crosslinking (CXL) was approved by the FDA in 2016, many individuals with KC have been encouraged to consider this treatment. While doctors are quick to point out that CXL is not a cure, in the majority of instances, disease progression halts and the resulting vision is no worse than it is on the day of surgery. For those who fear a lifetime of ongoing vision impairment, CXL is a welcome relief. Dr. Annie Nguyen MD , cornea specialist and Assistant Professor at the USC/Roski Eye Institute, has seen the value of CXL to her patients.
However, she notes, not everyone benefits from CXL. Here she names a few patient types who may not be good candidates:
The Stable or Older Patient : CXL is designed to be performed on those who have progressive KC. Dr. Nguyen notes that some individuals with mild cases can go their whole lives without knowing that they have KC. When they finally receive the diagnosis later in life, they are likely stable, having been ‘naturally crosslinked’ through a lifetime of exposure to UV light. Nguyen warns, “Patients over the age of 40 are unlikely to progress, however they should be monitored regularly. If progression is noted, these patients would be ideal candidates for CXL.”
The Scarred Cornea : Individuals may have scarring on their cornea – perhaps from some infection or condition that can disfigure the cornea including poorly fitting contacts or other trauma to the eye. If the cornea is scarred, and you undergo CXL, you may have stopped disease progression, but it will not do anything to improve impaired vision. Individuals with significant scarring, particularly in the central cornea, are often advised to consider a corneal transplant to provide a ‘clear window’ for their eyesight.
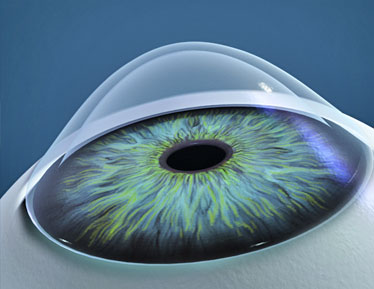
The Thin Cornea : If your cornea is too thin, your doctor may not be willing to perform CXL. A cornea should be at least 400 µm thick so that the riboflavin solution and UV-light used during the procedure does not cause damage to the endothelium (the bottom portion of the cornea). There are pharmaceutical solutions that your doctor can use to temporarily thicken the cornea for the CXL procedure. Researchers are experimenting with other modalities to help treat thin corneas, including using a contact lens when crosslinking.
The Post-Transplant Patient : Individuals with KC may believe that they would benefit from CXL, even after they have undergone a corneal transplant. When a doctor performs a corneal transplant, the weak, keratoconic tissue is replaced with a donor cornea and the need for CXL is usually eliminated.
The Cataract Patient : For individuals with progressive KC who have cataract, Dr. Nguyen recommends CXL first and then waiting until the cornea is stable (about six months) to proceed with the cataract extraction and placement of an intraocular len. For patients who have had cataract surgery previously, she will CXL if there are signs of disease progress. As with all decisions concerning CXL, the goal is to stabilize the cornea.
The Pregnant Patient : Since there is not research about the safety of CXL or the pharmaceutical solutions used during the procedure on unborn children or milk production, doctors will generally defer the procedure until after breastfeeding has ended. Women of child-bearing age who have progressive KC are encouraged to undergo CXL before they contemplate pregnancy.
The Squirmy Patient : Certain individuals may find they are unable to sit still for the procedure, or to fixate on the UV-light. While in a small minority of cases, this can mean that the procedure cannot take place, the doctor can usually offer a sedative to calm the uncooperative or extremely nervous patient. Patients with Down syndrome have a high rate of KC, and many doctors successfully perform CXL by having family members present during the treatment to help calm and direct patients. In some instances, CXL is performed under anesthesia.
In summary, Dr. Nguyen is a strong advocate for CXL for those who will benefit from the procedure. Yet not all individuals with a diagnosis of KC are ideal candidates. If your doctor recommends CXL for treatment of progressive KC, ask questions so that you understand how you will benefit from this procedure.
Dr. Annie Nguyen MD is a member of the Cornea Service at the USC/ Roski Eye Institute in Los Angeles. To arrange a consultation, visit eye.keckmedicine.org or call 323-442-6335.